This time it was Bucharest, the capital of Romania that hosted the HepHIV Conference 2019. Romania holds the EU presidency in the first half of 2019, and faces challenges in responding to the HIV, TB and viral hepatitis epidemics, in particular when it comes to addressing and including key populations in the response. In this sense, Bucharest was a good choice since the speakers could voice their concerns towards the Romanian Minister of Health and the local NGOs experienced a lot of support from the international community, in particular in the urgent call to the Romanian government to adopt the budget and implement the 2019-2021 National Strategic Plan for the surveillance, control and prevention of HIV/AIDS as soon as possible.
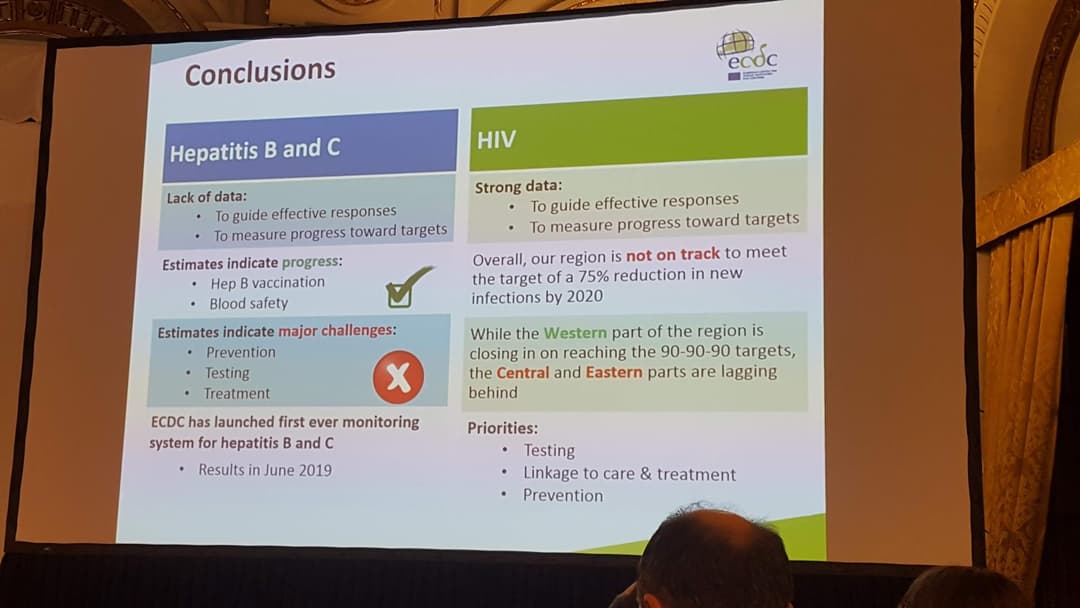
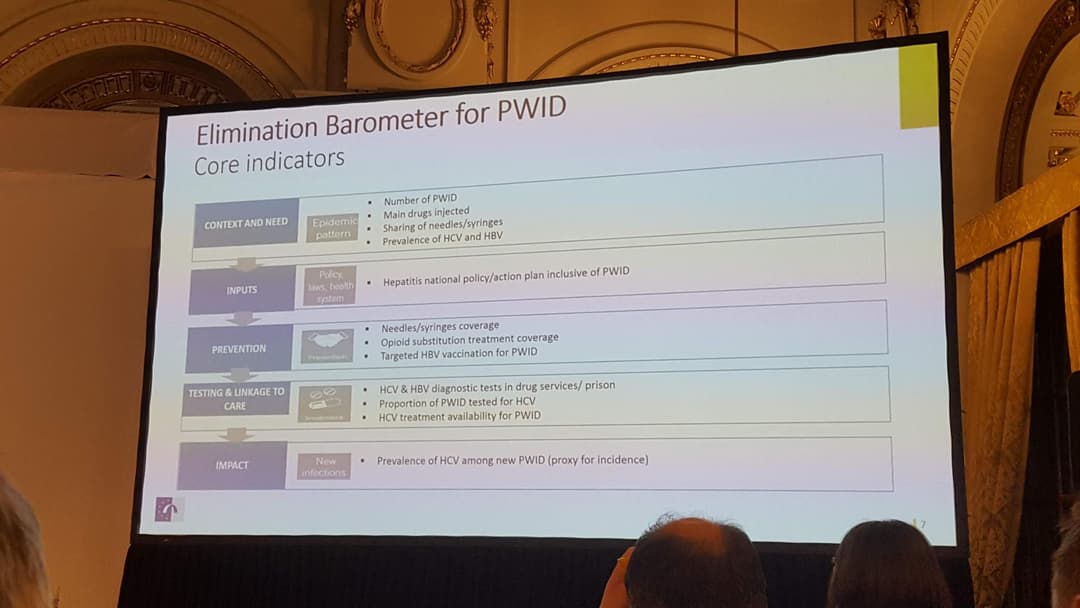
Apart from that – business as usual: recent surveillance data show again that the eastern European and central Asian countries are the only region globally where there is a growing HIV epidemic. While new HIV diagnoses in the European Union and European Economic Area (EU/EEA) show a steady decline of -10% in the past ten years the whole WHO European Region shows a drastic increase of +65% new HIV diagnoses. According to ECDC data, 131.000 new cases were reported just in the EAST of the WHO European Region [1] of Europe in 2017. Viral hepatitis surveillance remains challenging. However, it is obvious that if there is no immediate action to increase prevention and treatment of viral hepatitis, in particular of hepatitis B and C in people who use drugs, there is no way that the epidemic will be ended by 2030.
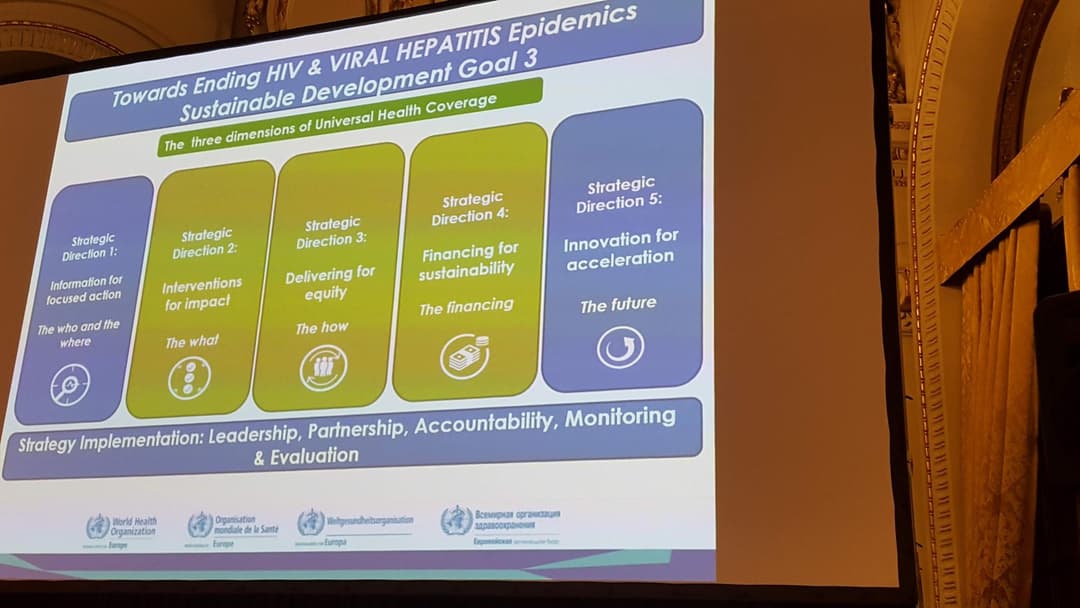
Testing for HIV, hepatitis B and C and linkage to care are the most important tools to reach the global targets. Moreover, and not new are the findings that community based approaches are badly needed to reach the populations most vulnerable, most affected and most stigmatised. Therefore, ECDC stresses again that embedding appropriate training and education programmes for healthcare providers and staff and involving lay providers into national testing strategies, including its monitoring and evaluation is absolutely vital.
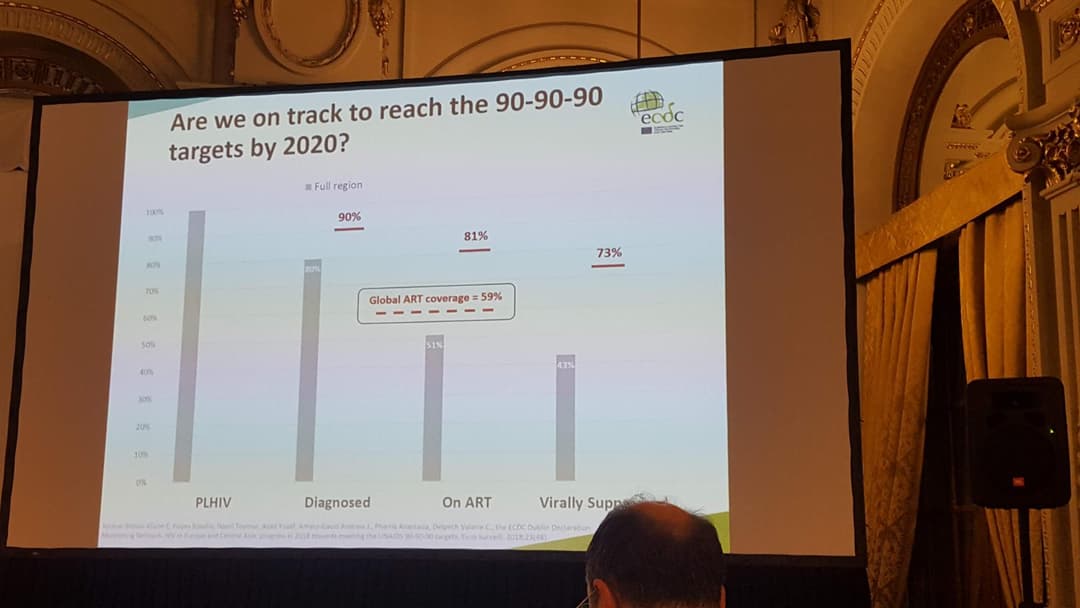
When it comes to reaching the UNAIDS 90-90-90 targets by 2020, the target most countries are struggling with is the target on diagnosis: 90% of all PLHIV know their status. Thus, there is a strong public health interest to trace and notify partners of those already diagnosed. However, these public health interests are in clear conflict with the human rights of the patients and bring up several issues around data protection and self-autonomy, especially in settings where criminalization and stigma and discrimination already deter people from getting tested if they are not underlying strict anonymization and voluntariness.
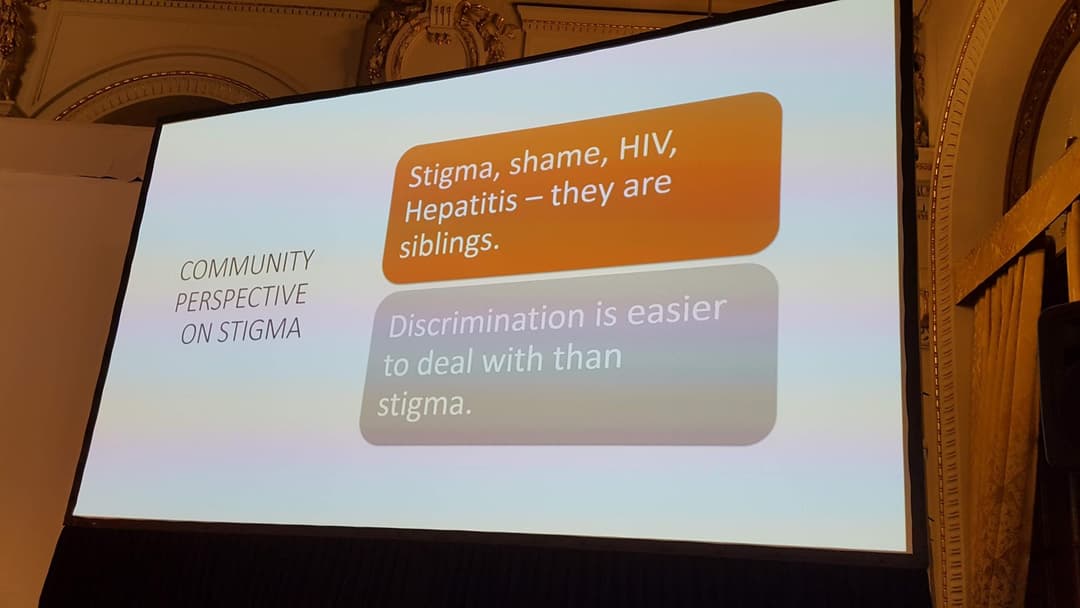
Stigma and discrimination challenges our daily life
The main obstacles – and again, this is not new either – are the exclusion of and the non-accessibility of services for whole groups of people due to discrimination and stigma. Sini Pasanen, Chair of AIDS Action Europe and co-Chair of the EU Civil Society Forum on HIV, viral hepatitis and TB, showed in her speech how stigma and discrimination challenge our daily lives and are obstacles to prevention, testing, treatment and care. We should acknowledge, work on and improve existing strategies to fight those obstacles in the healthcare system and beyond.
“Stigma seems to have its tentacles everywhere: HIV, different aspects of living with HIV, sex work, drug use, sexual orientation, sex and sexual behaviour… For example, why aren’t we still not ready to appreciate every person’s right to an age-appropriate, culturally relevant, scientifically accurate, realistic and non-judgmental information about sex and sexuality?
We need to understand the results when our actions are fuelled by stigma, not even to mention when actually discriminating or even criminalizing behaviours.
– Sini Pasanen, Chair of AIDS Action Europe and co-Chair of the EU Civil Society Forum on HIV, viral hepatitis and TB, Positiiviset ry, HivFinland
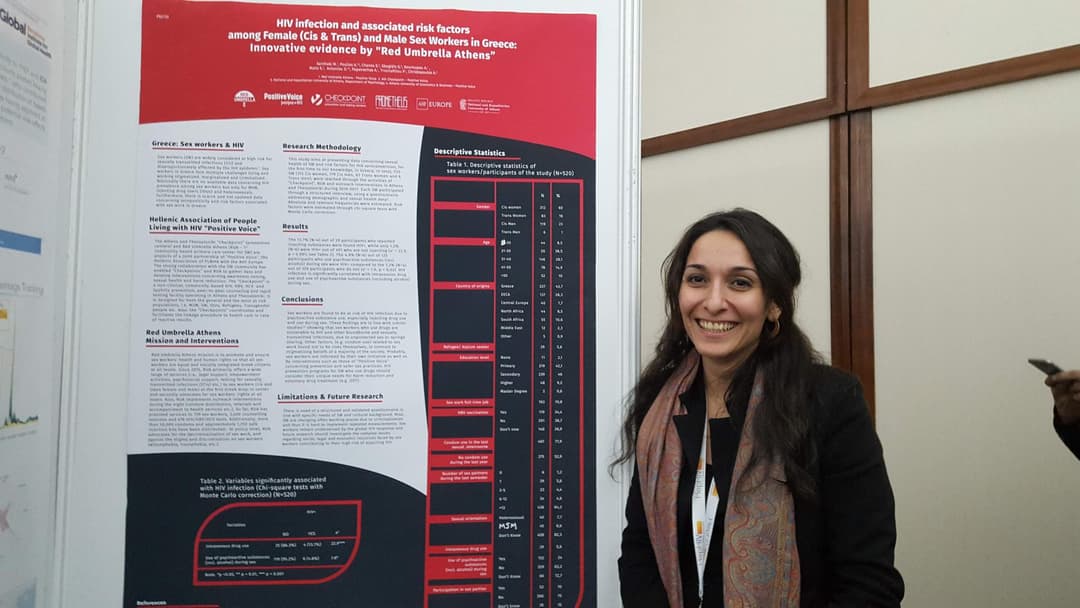
Maria Xanthaki from Red Umbrella Athens, points out that people who inject drugs, sex workers, homeless people, ex-prisoners, and undocumented migrants have increased vulnerabilities to HIV and hepatitis C infections and need improved healthcare services that are community-led and -based. Maria introduced the range of risk factors among sex workers in Greece, both female and male and both cis- and transgender, worked out by effective peer-led strategies by Athens and Thessaloniki Checkpoints and Red Umbrella. “The same applies to community based voluntary testing and counselling, which were proved an effective tool to get appropriate access to testing and treatment. “
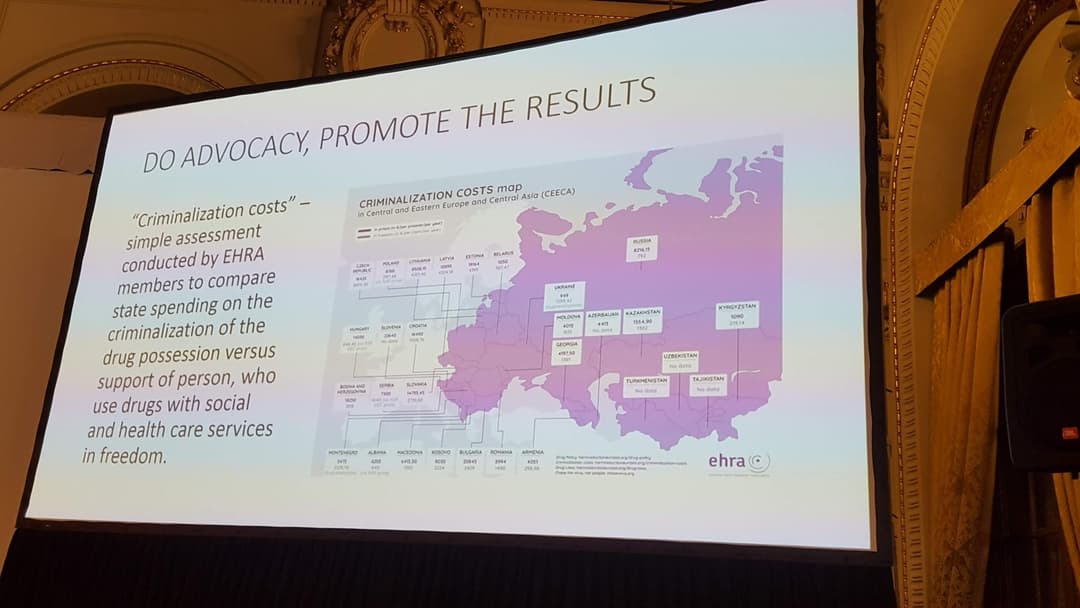
In addition to stigma and discrimination, criminalisation of HIV non-disclosure, exposure and transmission as well as the criminalisation of drug use or sex work increase vulnerabilities and limit accessing HIV and viral hepatitis services, thus increase of HIV and viral hepatitis transmission. The advocacy tool “Criminalization costs” – an assessment of state spending on the criminalization of the drug possession in CEECA countries prepared by EHRA – show how much money policy makers could save by endorsing harm reduction programmes and funding social and health care services for people who use drugs.
[1] HIV/AIDS surveillance in Europe 2018 - 2017 data - ECDC/WHO Europe